The Current19:05Calls for greater access to life-saving treatment for stroke
When Marleen Conacher was taken to a hospital for major stroke treatment for the second time in a week in 2021, she wasn't treated with a clot-busting drug like she was previously given at North Battleford Hospital in Saskatchewan.
Instead, she was transported directly to Royal University Hospital in Saskatoon, where a stroke team performed an endovascular thrombectomy (EVT).
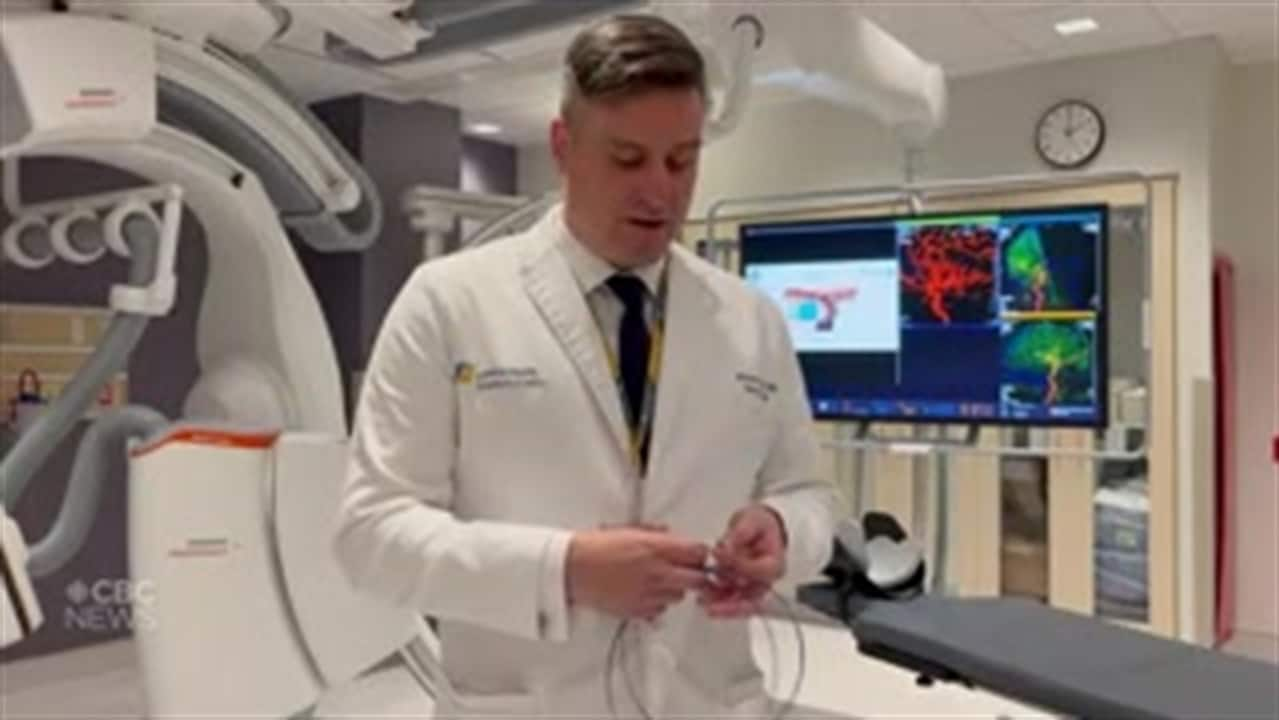
The procedure involved passing small devices through one of the arteries in her groin, and then using suction, or tubes called stents to pull the stroke-causing blood clot out.
"I don't recall when they, they put the little claw-like thing up through my groin and it went up through the artery and, and into my brain," she said. "But I do remember feeling when they had got to it and were pulling it out."
"It was a great deal of pressure. It did not hurt, but it was a great deal of pressure," she told The Current's Matt Galloway.
Within a few days of the stroke, Conacher was out of the hospital, walking on her own and ready to go shopping.
She said she doesn't think about the stroke much these days.
"I don't spend a lot of time, you know, thinking about having a stroke or whatever or that time," she said. "I just thank the good Lord that I am here."
EVT procedures are a relatively new option in the field of ischemic stroke treatment. In 2015, a study known as the escape stroke trial led by the University of Calgary's Hotchkiss Brain Institute found that, overall, positive outcomes for stroke patients increased from 20 per cent to 55 per cent thanks to EVTs.
Today, EVTs are used in about 25 to 30 major hospitals across Canada — and according to the senior study author and stroke specialist Dr. Michael Hill, it's had a "massive treatment effect."
"People would come in and they were paralyzed on one side, they couldn't speak or they were severely affected, and they were leaving the hospital in two or three days," he told Galloway.
"That was a visible change ... whereas [before] people would have stayed many days and weeks for their recovery and rehab, if they survived at all."
Speed is critical
Hill said the key to this procedure's success is speed, as "10 or 15 minutes makes a difference."
That's why a patient is often greeted at the door by a team of emergency department nurses, physicians and the stroke specialist.
"When we're alerted to a stroke or suspected stroke syndrome and we're meeting somebody in the emergency room, we're hustling to get there and be there before the patient or just after the patient arrives," said Hill, who is a neurologist at the Foothills Medical Centre in Calgary.
WATCH: Dr. Michael Mayich explains how clots that cause strokes can be removed
From there, medical personnel conduct a clinical and imaging assessment to confirm if a patient has a blood clot and where it may be.
If the clot is in a location that is "amenable to a vascular treatment," then an EVT will be offered.
Sedation can be approached in two ways, he said.
"Sometimes, patients are completely co-operative and we can do it completely awake. Sometimes they require some degree of sedation to keep them still."
"You can imagine it's important to do this procedure with your head relatively still. You can't have them thrashing around."

A game-changer
Hill said EVTs have a lot of potential in improving stroke treatment, as positive outcomes are a lot more frequent.
"So it's terrific, right? We get people back to their lives," he said.
In an ideal world, of course it's available everywhere because you don't have a stroke just because you live in the middle of Calgary or the middle of Toronto, right?-Dr. Michael Hill, stroke physician
At the moment, EVTs aren't available for all Canadians. Hill said the procedure is usually reserved for patients with the most severe forms of ischemic stroke, which occurs when the blood supply to part of the brain is interrupted or reduced.
"It's a tertiary-level procedure. You're not going to see it in a small, rural hospital," he said.
But part of that has to do with the volume of cases needed in order to develop expertise in this field, and it's big hospitals in major cities that tend to see the most patients.
"So if you're just doing one a year, you're more likely to have complications than you are to be successful," he said. "Whereas if you're doing 150 a year … everyone's ready for these things to occur because you're doing it so frequently."
Still, it's important to balance that expertise with availability.
"In an ideal world, of course [EVT is] available everywhere because you don't have a stroke just because you live in the middle of Calgary or the middle of Toronto, right?" He said.
For the time being, Conacher is content with how the procedure turned out — it's been nearly two years and the only major impact the stroke has had is a bit of memory loss.
Furthermore, as someone who saw her dad suffer paralysis in his left side due to stroke, she's pleased with the way stroke treatment is evolving.
"If they had things like this, I think he would have been just as fine as I was," she said.
Produced by Ines Colabrese.
New stroke treatment helps more Canadian patients return home to their normal lives - CBC.ca
Read More

No comments:
Post a Comment