The prevalence of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) continues to increase, compounded by risk factors such as advanced age, obesity, ethnicity, and type 2 diabetes mellitus (T2DM). As NAFLD progresses to NASH, the same factors also contribute to liver fibrogenesis (abnormal accumulation of fibrous tissue). Constant liver damage results in progressive scarring (fibrosis), which disrupts the structural integrity of the liver through fibrosis bands, parenchyma nodules, and blood vessel abnormalities, leading to cirrhosis. Hence, liver fibrosis is a key criterion that represents the severity of liver illnesses and is an important factor that helps physicians forecast the progression of liver disorders towards cirrhosis.
Although liver biopsies are currently considered to be the gold standard for the diagnosis and histological assessment of NAFLD/NASH, they are not without limitations (Li et al., 2022; Zeng et al., 2022). In addition to being a costly and invasive procedure, the estimated number of patients with NASH vastly outnumbers the number of specialists with the proper skills and expertise to perform and interpret a liver biopsy. Additionally, liver biopsies are prone to sampling errors, as fibrosis is not uniform throughout the liver, making it difficult to distinguish between the stages of fibrosis. As such, there has been much interest in developing non-invasive tests (NITs) to detect markers of fibrosis. These NITs are usually categorised based on the test’s modality, such as imaging or serum blood tests, or components like direct markers versus indirect markers of fibrosis.
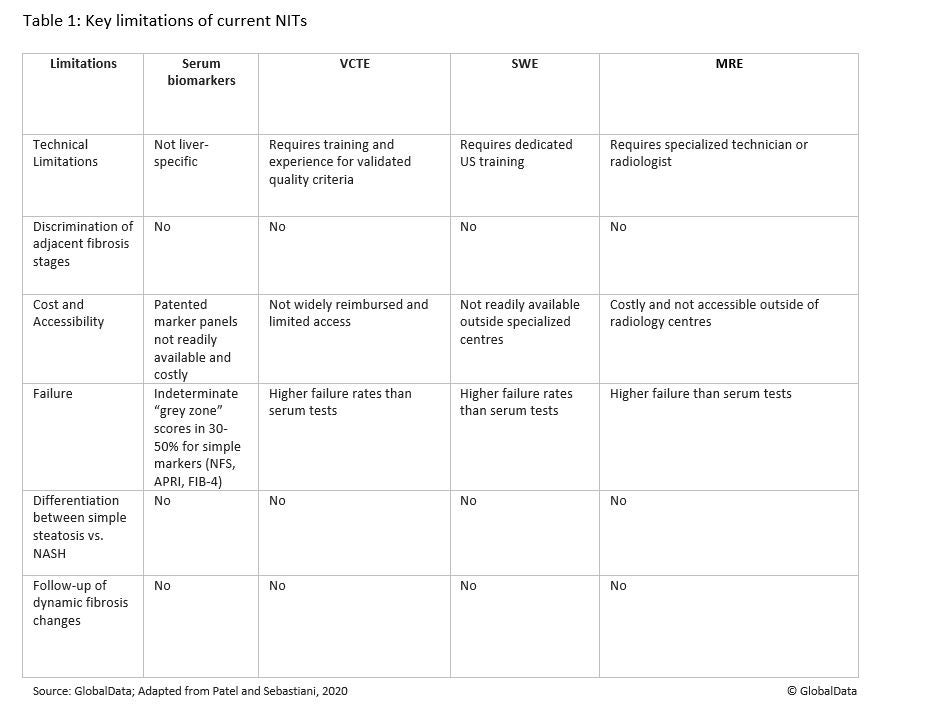
Serum biomarkers identified via multi-biomarker panel blood tests and non-invasive imaging tests such as transient elastography (VCTE), shear wave elastography (SWE), and magnetic resonance elastography (MRE) can be used to identify patients with liver steatosis, determine the stage of fibrosis, and diagnose NAFLD/NASH. While non-invasive imaging and serum blood tests are cost-effective, accessible, and have high reproducibility compared to a liver biopsy, they also have limitations. Table 1 highlights some of the key limitations of current NITs.
Despite these limitations, the American Association for the Study of Liver Diseases (AASLD) recently published its 2023 NAFLD Practice Guidance to suggest the use of vibration controlled transient elastography (VCTE), a patented technology used by Echosens’s FibroScan for detecting and diagnosing NAFLD in high-risk individuals, including those with type 2 diabetes. FibroScan is a non-invasive device that assesses the ‘hardness’, or stiffness, of the liver via transient elastography, an ultrasound-based technology.
However, with the possibility of the first set of approvals for NASH therapies coming soon, data on the performance of NITs being used in current Phase III clinical trials could help address their limitations for diagnosis and treatment monitoring in NASH. In addition to making the diagnosis process more economic and accessible, the use of NITs in lieu of a liver biopsy could help shape the future treatment paradigm of NAFLD/NASH.
Li, G., et al. (2022) ‘Non-invasive tests of non-alcoholic fatty liver disease’, Chinese Medical Journal, 135(5), pp. 532–546. Available at: https://ift.tt/ub2kPvG
alcoholic_fatty_liver.7.aspx (Accessed: 22 February 2023).
Patel, K. and Sebastiani, G. (2020) ‘Limitations of non-invasive tests for assessment of liver fibrosis’, JHEP Reports, 2(2). Available at: https://ift.tt/P4xJita (Accessed: 22 February 2023).
Zeng, Y., et al. (2022) ‘Advance of serum biomarkers and combined diagnostic panels in nonalcoholic fatty liver disease’, Disease Markers. Available at: https://ift.tt/bZx3oNW (Accessed: 22 February 2023).
The future of diagnosing and monitoring NAFLD/NASH could be noninvasive - Pharmaceutical Technology
Read More

No comments:
Post a Comment