
Two mothers who died of herpes after giving birth could have been infected by a single surgeon, the BBC has found.
The doctor performed Caesareans on both the women in 2018.
The families, who were told there were no connections between the deaths, are calling for inquests to be opened.
The East Kent Hospitals Trust says it could not identify the source of the infection, and the surgeon had no history of the virus.
Maternal deaths are rare. In more than 2.1 million births in the UK between 2017 and 2019 there were 191 deaths of mothers within six weeks of giving birth, according to official figures.
Deaths caused by HSV-1 - one of two strains of the herpes simplex virus - are almost unheard of in healthy people. It is a common infection that can cause sores around the mouth or genitals.
Yet, in May and July 2018, two young mothers died from an infection caused by the virus.
The BBC has been investigating how these two deaths happened and why neither family was told there was a link between them.
Kimberley Sampson, 29, a barber, lived with her three-year-old daughter at her mother's home in the seaside town of Whitstable in Kent.
"She was fun, she was loving, and she had lots of friends," her mother Yvette Sampson tells the BBC. "She was a brilliant mummy and that's what she wanted to be."
Kimberley's pregnancy progressed smoothly and on 3 May 2018, she went on to the labour ward of the Queen Elizabeth the Queen Mother Hospital in Margate.
"She thought everything was going to be fine," says Yvette. But things started to go wrong. Her labour was not progressing quickly, her mother says, and Kimberley kept saying the baby was stuck.
Eventually, doctors decided to perform a Caesarean - also known as a C-section - where a baby is delivered through cuts in a woman's abdomen and uterus.
Her son was delivered, but Kimberley needed a blood transfusion because she sustained injuries during the operation. After two days, she asked to be discharged with her baby. But she was in a lot of pain and despite being barely able to walk, she left the hospital with her mother.

But the pain became worse. Even a gentle touch was enough for her to scream in agony, says Yvette.
"She deteriorated day after day - she couldn't eat, she couldn't sleep."
Her GP suggested they call 999 and Kimberley was taken back to hospital in an ambulance. Doctors thought she was suffering from bacterial sepsis - a potentially very serious condition. She was sent back to the maternity ward and given antibiotics. They didn't work and her condition worsened.
A series of operations followed as doctors struggled to identify and treat the infection. Eight days after she had been readmitted to hospital a consultant microbiologist suggested trying the antiviral drug Aciclovir - which is used to treat herpes infections.
Kimberley was transferred to Kings College Hospital in London, where she was diagnosed with a catastrophic herpes infection.
While she was in intensive care, Yvette says she was told her daughter only had "hours or days".
On 22 May, Kimberley died.

One death from herpes is rare enough, but just six weeks later, Samantha Mulcahy would die of the same condition.
The 32-year-old nursery nurse lived with her husband, Ryan, 20 miles (32km) from Kimberley.
The couple had been together since they were teenagers. Ryan had first spotted her when working a part-time job at his local Tesco, but it took him months to get up the nerve to ask her out.
Samantha's mother, Nicola Foster, says her daughter was excited about being pregnant with her first child. "I think she was already talking about having more children."
But what should have been a joyous time for them turned into a tragedy. Samantha went into labour four weeks before her due date, and in July 2018 went into the William Harvey Hospital in Ashford - which is run by the same Trust as the hospital where Kimberley's baby had been delivered.
After 17 hours of contractions and pushing, she was exhausted and in pain.
After some worrying blood test results, she was taken for a Caesarean section. Her daughter was born healthy, but because doctors were concerned about signs of the blood pressure condition pre-eclampsia, they decided to keep Samantha in for observation.
After three days her condition began to deteriorate - despite no longer showing signs of pre-eclampsia. Her stomach became swollen, she had a temperature, and her blood pressure was raised.
Samantha became so swollen that her mother said it looked like she had "elephant's legs". Like Kimberley, doctors thought Samantha was suffering from bacterial sepsis. She was also given antibiotics, but they didn't work.

As her condition worsened rapidly, her organs began to shut down. She was taken to intensive care where she stayed for four days.
At one stage, a doctor suggested she be treated with antiviral medication, but they were advised by the microbiology department to continue with antibiotics instead.
Doctors called for support from a hospital in London, and surgeons took her into the operating theatre to try to stabilise her.
"They told us that unfortunately they couldn't save her," says Nicola. "That she'd gone. Passed away."
The post-mortem investigation found Samantha had died from multi-organ failure following a "disseminated herpes simplex type 1 infection".
In other words, an overwhelming infection caused by the HSV-1 virus.
Neither woman's baby was found to have been infected with the virus.
Both women had what is known as a primary infection - meaning that this was the first time they had been infected by herpes.
Hospital analysis of the women's medical history indicates they'd not previously had herpes, so they would have had no antibodies - or natural protection - against the virus. This, combined with the fact that women in late stages of pregnancy have reduced protection from their immune system, would have made them more vulnerable to a serious HSV infection.
- Herpes viruses are generally passed on by skin-to-skin contact with someone with the virus
- Herpes infections are common with almost 70% of adults having one of the two types of the virus by the time they are 25
- Some people will develop cold sores or genital herpes, but about two-thirds will have no, or mild, symptoms
Source: Herpes Viruses Association
More than a year after the women's deaths, the families each received a letter from the coroner, Katrina Hepburn, saying there would be no inquests in these cases. The letters acknowledged there had been a similar case but said there was "no connection" between the two deaths. They also set out the belief of the pathologist who investigated both deaths, that the women had been infected with herpes "prior to hospital admission".

BBC News began investigating the East Kent Hospitals Trust's maternity department in 2019, ahead of the inquest of baby Harry Richford, whose death was determined to be "wholly avoidable" by a coroner.
We found further cases of preventable baby deaths at the Trust, and a government-ordered review of maternity services is under way.
BBC News became aware of the deaths of Kimberley Sampson and Samantha Mulcahy at the same Trust in the spring of 2021, and has worked closely with the families to try to find out what happened to them.
While reviewing documents sent to the families, we noticed that Public Health England (PHE) had looked into the possible source of the herpes viruses. But no detail had been provided.
The family of Kimberley Sampson subsequently made a request to PHE for access to that investigation. It reveals documents which cast new light on the two deaths and show, for the first time, the significant link between the two cases.
Among them are two email chains between staff at PHE, the East Kent Hospitals Trust, some NHS bodies and a private lab called Micropathology.
They show the efforts that went into trying to establish how the women became sick, whether the two viruses were genetically identical, and whether they could have come from a common source.
The emails were partly redacted by Public Health England to hide the names of those involved.
In one of them, someone from the Trust reveals that the same two clinicians had taken part in the deliveries of both Kimberley's and Samatha's babies - a midwife and the surgeon who carried out their Caesarean sections.
This apparent connection - and possible source of infection - caused concern among the people on the email chain.
The private lab Micropathology was brought in to try to sequence the genome of the two viruses - to see if they were the same.
In an email sent a fortnight after Samantha died, someone working for the lab says both cases "look like surgical contamination" and asks the Trust to provide "a mouth swab/lesion swab from the suspect surgeon in O&G".
We know the Trust did not provide these samples, and none of this information was passed to either of the families at the time.
The emails also show that the parts of the virus that were tested were identical.
In an email sent in October 2018, a Micropathology worker says "it seems the most likely explanation [is] that these strains are probably the same… which also adds weight to the idea that these two women were infected with the same virus."
An email from a member of staff from Public Health England just over a year later says the type of virus was "rare" compared with the previous 10 years of herpes virus samples collected at its lab in north London.
This shows the investigation was continuing after the families received the letter from the coroner denying them inquests.
The BBC asked Peter Greenhouse, who has worked as a consultant in sexual health in the UK for almost 30 years and has a particular interest in the herpes viruses, to review the cases.
He describes them as "very unusual - very rare indeed".
He says "you can never be 100% certain what happened in these cases", but "from all the evidence that we have it's very unlikely that they acquired [the virus] before they got into hospital" - contradicting the position of the pathologist.
"It is more likely that they picked it up in the hospital and less likely that they picked it up in the community, or sexually, because there were no facial or genital lesions - obvious or even hidden signs - whatsoever."
After reviewing the documentation uncovered by the BBC, Mr Greenhouse has developed a theory for what might have happened.
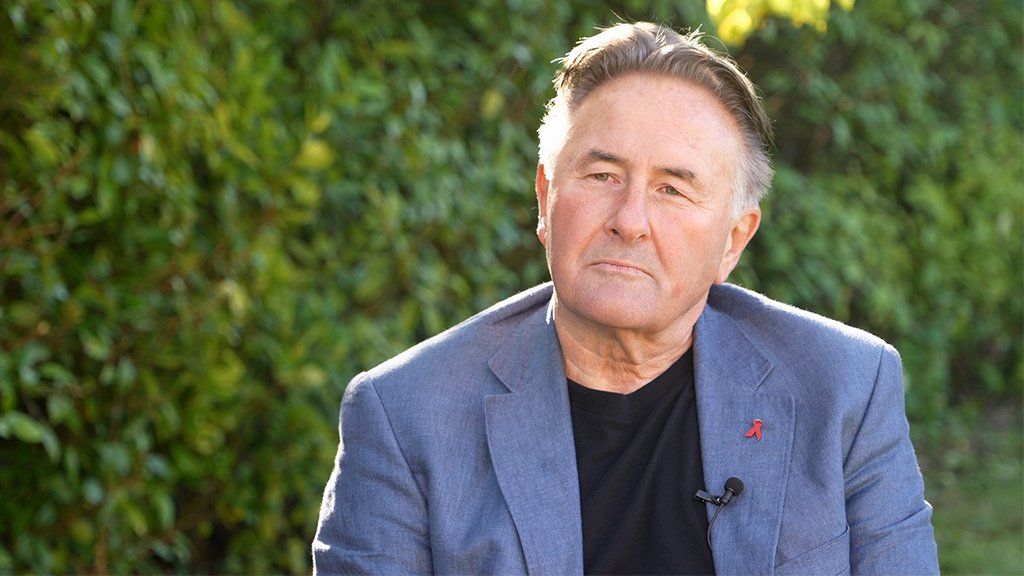
He believes it is most likely that the infection may have been given to the two women accidentally by the surgeon during the Caesarean section.
"The only common source here, in a hospital-based scenario, would be the surgeon who performed the operations," he says.
He says it is possible the surgeon may have had a herpetic whitlow - a herpes infection on the finger - which could have "directly seeded the herpes into the abdomen of the women".
This, he says, would have allowed it to spread throughout the abdomen quickly and explains why the women had no external lesions, which you would normally expect to see with a herpes infection.
According to the NHS website, the symptoms of a whitlow can vary from a small bump to open lesions - meaning they can go undetected.
"Many of these will occur without any obvious signs, or they'll be so miniscule that you can't identify them," says Mr Greenhouse.
All surgeons wear gloves during surgery, but Mr Greenhouse says it might have been possible that they split during the operations allowing the virus to spread.
A small study in 1990 suggested as many as 54% of gloves used in Caesarean sections had holes in them when they were tested with water after the operations.
Further experiments following other forms of surgery produced similar results.
"It's a very rare but a very biologically plausible method of transmission," Mr Greenhouse explains.
Four other experts in sexual health and virology have backed up Mr Greenhouse's theory.
In a statement, the East Kent Hospitals Trust says the surgeon underwent a verbal Occupational Health check where he said he had no history of herpes infection and had no hand lesions, although he was not tested for the virus at the time of the operations.
Referring to the email stating that the type of virus was "rare", compared with other samples collected at PHE's lab, Mr Greenhouse says this makes the likelihood that the women were infected by a common source in the hospital more likely - and much less likely they were infected in the community.
The East Kent Hospitals Trust points out that PHE's report says although there was a "high probability they are epidemiologically linked" for HSV "this finding does not mean that the viral isolates have an immediate common source or are part of a transmission chain".
The families of the two women have been calling on the coroner to open inquests into the deaths.
Yvette Sampson says it's important for the children who've been left without their mother - "when they're a bit older they're going to need to know why their mummy died".
In a statement Dr Rebecca Martin, Chief Medical Officer for East Kent Hospitals, said:
"Our deepest sympathies are with the families and friends of Kimberley and Samantha.
"East Kent Hospitals sought specialist support from Public Health England (PHE) following the tragic deaths of Kimberley and Samantha in 2018. The investigations led by the Trust and the Healthcare Safety Investigation Branch took advice from a number of experts and concluded that it was not possible to identify the source of either infection.
"The surgeon who performed both Caesarean sections did not have any hand lesions that could have caused infection, or any history of the virus.
"Kimberley and Samantha's treatment was based on the different symptoms showed during their illness. Our thoughts are with their families, and we will do all we can to answer their concerns."
Peter Greenhouse is now carrying out further research into the deaths - in the hope that it might mean new mothers with unexplained sepsis-like symptoms will be tested for herpes as a matter of course.
"I hope that the research will eventually change the guidelines, so more people will benefit from earlier diagnosis. It is the only constructive outcome that one could hope for, after such a tragic scenario."
New mothers who died of herpes could have been infected by one surgeon - BBC News
Read More

No comments:
Post a Comment